RX 590 first evaluation: the new technology has not improved much, but it is enough to hang 1060.
[PConline first evaluation]This year’s DIY hardware market is not very friendly to gamers. First of all, the mining tide at the beginning of the year led to the soaring price of graphics cards. Finally, the mining tide faded and Intel’s so-called 14nm capacity crisis occurred, and the price of CPU began to soar. The price of NVIDIA’s new RTX graphics cards was even more expensive. When the price of Intel CPU soars, we can choose AMD Ryzen processor, which is more affordable, as a substitute. Then, when the price of NVIDIA soars, we naturally hope that AMD can come up with better new products to make us feel refreshed. It’s not, RX 590 is coming.
Today, AMD officially released a brand-new RX 590 graphics card. Today, let PConline Jia Xiaobin take you to see if this new graphics card can undertake the sacred task of saving the majority of DIY players.
Under normal circumstances, there will be a large section of technical analysis about the product in the first test, but not this time, because the RX 590 will not have too many innovations, and we can summarize it from several aspects.
First, the graphics card still adopts Polaris architecture, and the core code is Polaris 30.
Second, the number of stream processors for graphics cards is still 2,304, which means that the specifications of RX 590 are the same as those of RX 580, which may not be in line with our cognition. After all, the specifications of AMD graphics cards will be improved compared with those of ~90 models, but this is the reality.
Third, the graphics card uses Grofonde’s latest FinFET 12nm, which should be the same technology as the second generation Ruilong. Judging from the performance of the second generation Ruilong,GF’s 12nm process can improve the overclocking ceiling of the core and reduce the power consumption of the same frequency.Let’s see if this is the case in the following test.
Fourth, the video memory of the graphics card is 8GB, and the GDDR5 video memory is still used.
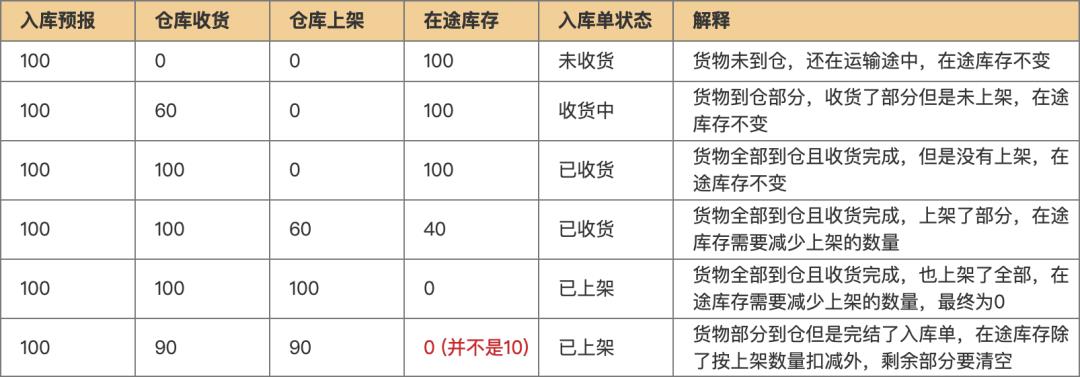
From the comparison of the following tables, we can see the difference between RX 590 and RX 580 and RX 480 more intuitively.
From 1999 yuan (8GB)
Parameter comments:Because the Polaris 20 core used by RX 580 is already a complete body of Polaris architecture, there is no room for increasing specifications. Therefore, the adoption of Polaris architecture by RX 590 also means parameters such as stream processor and texture unit of graphics card.And RX 580 are exactly the same., but using a better process to Refresh the core, so the improvement of frequency and the change of power consumption have become the biggest differences of RX 590, which are also the focus of this evaluation.
This is the same routine as the upgrade of RX 580 compared with RX 480. Simply speaking, RX 590 is a duplicated version of RX 480.The difference is that RX 580 uses the same process as RX 480, but the process is more mature and allows AMD to overclock, while RX 590 uses a brand-new 12nm process, and the frequency progress is also relatively large.
To be honest, Xiaobian is still a little disappointed with the parameters of RX 590. Although the frequency of RX 590 is 205MHz higher than that of RX 580, it is about 15%, but when the graphics card specifications are unchanged,With the increase of frequency, the performance of graphics cards will increase less and less.Just like the so-called barrel theory, how much water can be loaded depends on the short board of the barrel.
The starting price did not increase, and it remained at the same 1999, which is good.
Considering the huge performance gap between GTX 1070 and GTX 1060, it seems impossible for RX 590 to challenge GTX 1070 this time. Is this the case? Don’t worry, the later on-board measurement can solve your doubts.
This time, RX 590, like RX 580, is also the first launch, and it is directly released in a non-public version. This time, we also got a non-public version of the sapphire RX 590 Ultra Platinum Aurora Special Edition, which is also the protagonist of this RX 590 evaluation.

The appearance of the graphics card is basically the same as that of RX 580 Ultra Platinum Aurora Special Edition, with the ancestral "gas stove" shape, but the graphics card is dominated by light blue color matching and decorated with a little gray, which makes the square graphics card look very energetic and no longer rigid.

The video card fan is an LED fan with a diameter of 95mm, and its blades are transparent, which makes it easy to transmit light when starting. At the same time, the video card fan is designed to be detachable, so consumers can replace it themselves when they don’t like light pollution or the fan is faulty.

There will be a sapphire RGB belief light at the top of the graphics card, which supports 6 modes.

The external power supply of the graphics card is designed as 8+6pin, which is consistent with the RX 580 Ultra Platinum Aurora Edition.


The thickness of the graphics card is about 2.2 slots, and it is filled with very dense fins, which is a good material in the mid-range graphics card, which also shows that the heat of the graphics card should be considerable.

The graphics card also has a large area of backboard, and the backboard is mainly light blue. The large area of backboard can not only play a protective role, but also assist the graphics card to dissipate heat.

The graphics card also has two BIOS, and the mute BIOS is close to the video output interface.The core frequency is 1545MHz consistent with the public version, the video memory frequency is 8000MHz, and the other side is the game BIOS, with the core frequency of 1560MHz and the effective video memory frequency of 8400MHz.

The video output interface of the graphics card is designed as 2 HDMI+2 DP+1 DVI.

It is not difficult to disassemble the graphics card. Just unscrew all the screws on the back plate with a moderately sized Phillips screwdriver. The heat dissipation material of the graphics card is still good. The part in direct contact with the GPU uses a pure copper base, and the parts in contact with the video memory and power supply are also covered with heat conduction stickers.

The graphics card uses 4 heat pipes, 2 8mm and 2 6 mm.

Next, look at the PCB board of the graphics card.

This is the high-definition codeless recent photo of Polaris 30 core.


The core size is about 14 mm * 18 mm.

The memory comes from magnesium light, with a single capacity of 1GB, a total of 8.

The power supply of the graphics card is designed as 6+1+1, and the fourth generation black diamond inductor and 16K black gold capacitor are used to ensure the stability of the power supply of the core and video memory.
The disassembly of the graphics card is here. Let’s carry out the on-board measurement that everyone is most concerned about.
The platform collocation of graphics card test is very important. The following is the test platform used in the initial evaluation of RX 590.
NVIDIA GTX 1060 6GB Founders Edition
Asus DUAL RX580 O8G
Sapphire RX VEGA 56 Ultra Platinum Limited Edition
Asus dragon knight DRAGON GTX1070 TOP8G
AMD: 18.10.2(RX 580&RX VEGA 56)
18.8.1(RX 590)
3DMark Frie Strike URLRA
3DMAark TIME SPY
Extreme Racing: Horizon 4
Singularity ashes
Strange squad
Assassin’s Creed: Odyssey
Whole territory blockade
In order to ensure that the CPU and memory of the platform will not become bottlenecks, we all try to use high-standard hardware. Although the i7-8700K is the flagship of the previous generation, it is more than enough to squeeze out the performance of the mid-range graphics card, and the memory of 3200MHz is also luxurious for the mid-range installed configuration.
The above is the information displayed by the sapphire RX 590 Ultra Platinum Aurora Special Edition in GPU-Z. Because GPU-Z has not been updated, some information is displayed incorrectly, such as the process or the 14nm process.
Because the sapphire RX 590 Ultra Platinum Aurora Special Edition uses mute, the frequency of the graphics card is exactly the same as that of the public version.Therefore, we also use silent BIOS for testing, which can be directly regarded as the performance of RX 590 public version.
GTX 1060 uses the public version. There is nothing to say. RX 580 uses ASUS DUAL RX 580 O8G.Because its frequency is 1360MHz, it is very close to the public version, and its performance is about 1~2% different from that of RX 580, which can basically be regarded as RX 580 public version..
The GTX 1070 was close to production stop a long time ago, so it was difficult to find this graphics card, and the evaluation room could only find this ASUS DRAGON GTX 1070 TOP8G. It is worth noting that the frequency of this GTX 1070 has reached 1671MHz, and the nominal maximum frequency is 1874MHz (of course, the actual BOOST frequency of the N card is definitely much higher than this), which is 11% higher than that of the public version.It is one of the strongest GTX 1070 non-public versions, and its theoretical performance is 6~8% stronger than that of GTX 1070 public version.Of course, the power consumption of the graphics card will be about 40w higher, so you want to know the performance gap between the RX 590 public version and the GTX 1070 public version in the following test.Properly reduce the performance of GTX 1070 in the test..
The situation of RX VEGA 56 is similar. We only found the sapphire RX VEGA 56 ultra-platinum limited edition as the test graphics card, but we used the silent BIOS of the graphics card.The performance is 2~4% better than that of RX VEGA 56 public version.The power consumption is about 30w higher.
First, the theoretical test of 3DMark, in addition to the two commonly used tests of FireStrike Extreme and FireStrike Ultra, there is also the Time Spy of DirectX 12 benchmark performance test for game PC launched by 3DMark. At the same time, in order to ensure the beauty of the chart, the name of the graphics card is omitted.
Summary of theoretical performance test:In the end, sapphire RX 590 is 12%, 14% and 11% stronger than ASUS RX 580 in the three tests, which is not a big improvement, but the gap is not small.
Compared with the GTX 1060 public version, it is 17~22% stronger, and compared with the ASUS DRAGON GTX 1070 TOP8G, it is about 22~28% behind, not to mention the sapphire RX VEGA 56 ultra-platinum limited edition.
Simply put, the theoretical performance of RX 590 should be just inserted between GTX 1060 and GTX 1070..
However, 3DMark can only measure the theoretical performance of the graphics card after all, and how many game frames the graphics card can bring is what we are most concerned about. Let’s measure the game below. There are 6 games we tested, including the latest and most popular 3A masterpieces Assassin’s Creed: Odyssey, Tomb Raider: Shadow and Extreme Racing: Horizon 4, as well as the game Singularity Ashes, which Microsoft used to promote DX12′ s own operation. The test results are very representative.
1. Tomb Raider: Shadow

Unconsciously, Laura has been with us for 20 years, and has developed into the 11th generation. Today, she has been able to support all kinds of latest, true and most eye-catching graphics technologies.
2. Extreme Racing: Horizon 4

As an old racing game, forza motorsport series is very famous. This series is made by Playground Games. The open world of this series is the biggest highlight different from the original series. It is known as "the best racing game in this century", and its picture quality is exquisite and optimized. Netizens who like racing must not miss it.
3. Assassin’s Creed: Odyssey

Assassin’s Creed: Odyssey is the 11th work in the Assassin’s Creed series, which was created by Ubisoft. In the game, players will return to ancient Greece and play a mercenary with Spartan ancestry who was sentenced to death by his family, thus starting an epic journey from a young abandoned man to a legendary hero. The plot design and image quality of the game are very brilliant, and it is a strong competitor for the best game of the year.
4. "Singularity Ash"

Microsoft’s personal work to promote DX12 API perfectly supports all the effects of DX12. Benchmark optimization is in place, and it is also very suitable for testing DX12 performance and graphics performance of graphics cards.
5. Strange Squad

"Strange Squad" is also a new game that went on the market only at the end of August. The PC started and supported DX12 perfectly, and the Steam list was highly rated.
6. "Whole Territory Blockade"
It is also a classic masterpiece created by Ubisoft, which is all the rage. It is said that the second one will come out soon, and then our evaluation room will test the game with the new version.
Summary of game evaluation:The improvement of RX 590 compared with RX 580 is obvious. At 1080p, it can generally improve about 7 or 8 frames. In many games, it can be improved from "playable" to "fluent 60 frames", which is not bad. We summarize the performance of five graphics cards in six games under 1080p, and get the following chart.
At 1080p, sapphire RX 590 Aurora Special Edition can lead GTX 1060 public edition by about 14% and ASUS DUAL RX 580 O8G by about 13% on the frequency of public edition. However, the RX 590 is still about 25% behind the ASUS DRAGON GTX 1070 TOP8G, and about 35% behind the sapphire RX VEGA 56 ultra-platinum limited edition.
When it comes to 2k resolution, because A card has always been willing to allocate video memory, the bandwidth of video memory of A card at the same level will be larger than that of N card. The higher the resolution, the better the performance of A card in comparison, and this time is no exception. At 2K resolution, RX 590 is 20% ahead of GTX 1060, and about 23% behind ASUS DRAGON GTX 1070 TOP8G.
Since it is impossible to test the power consumption of a certain hardware separately, the following are all the power consumption of the whole machine, which are three application scenarios. The game is fully loaded with the peak power consumption of the whole machine in the 11》Benchmark process of Tomb Raider 11, and the graphics card is fully loaded with the peak power consumption of the whole machine in the 3DMark stress test.
Power consumption has always been the most disadvantage of A card. From the results, A card really can’t reach the excellent energy efficiency ratio as N card, and the gap is not small. The platform power consumption of RX 590 is about 100w higher than that of GTX 1060, and 30~40w higher than that of high-frequency GTX 1070.
We mainly look at the new technology to make the new AMD graphics card compare with the old one. From the results, the power consumption of RX 590 with public version frequency is still higher than that of RX 580 with public version frequency, which is about 40 W. Does this mean that GF’s 12nm process is useless?
We also found the sapphire RX 580 ultra-platinum limited edition as a comparison. The sapphire RX 580 ultra-platinum limited edition is the highest frequency RX 580, reaching 1450MHz. From the results, the platform power consumption of sapphire RX 580 Ultra Platinum Limited Edition is basically the same as that of sapphire RX 590 Ultra Platinum Aurora Special Edition, and even the RX 590 platform is slightly lower.However, the frequency of the sapphire RX 590 Ultra Platinum Aurora Special Edition is 95MHz higher.
That is to say, GF’s 12nm technology can increase the power consumption of graphics cards by about 100MHz.Looking at the new technology in this way is not a gimmick, it is indeed an improvement. In fact, we probably know how much progress GF has made at 12nm from the performance of the second-generation Ruilong compared with the first-generation Ruilong, and the GPU core is larger, which makes it more difficult to improve the frequency. We can only say that the performance of this process is in line with Xiaobian’s expectations, and there is progress, but the improvement is not great.
Let’s take a look at the performance of sapphire RX 590 Ultra Platinum Aurora Special Edition in terms of temperature, noise and stability. The test performance of this graphics card is closely related to the design and manufacturing skills of sapphire graphics cards.
3DMARK stress test results:
In the 3DMark stress test, 97% passed, and finally the graphics card passed the test with a score of 98.6%, indicating that the stability of the graphics card is no problem. In the stress test, the highest instantaneous frequency of the graphics card is 1514MHz, which does not reach the nominal value of 1545. It may be limited by TDP. Click on the picture to see the specific value.
Summarizing the stability performance of the tested graphics cards, the performance of sapphire RX 590 Ultra Platinum Aurora Special Edition is quite good, which reflects the basic skills of sapphire graphics card manufacturing.
Full load temperature test:
In fact, the 3DMARK stress test just now also showed this temperature performance.
Although the heat dissipation material of the graphics card is very willing, RX 590 is indeed a big fever. Finally, the full-load temperature of the graphics card still reaches 75 C, but this temperature is OK, and the difference of several degrees Celsius will not obviously affect the user experience.
Noise test:
The noise of the graphics card is 54 decibels, which belongs to a quiet level, and the noise control of the graphics card is quite good.
About noise:
0-20 decibels: very quiet, almost imperceptible; 20-40 decibels: quiet, like whispering; 40-60 decibels: general indoor conversation; 60-70 decibels: noisy: harmful to nerves; 70-90 dB: It is noisy and nerve cells are destroyed. 90-100 decibels: increased noise and hearing loss; 100-120 decibels: unbearable, temporarily deaf after staying for one minute. Above 120 decibels: extremely deaf or totally deaf; About 300 dB or above: 20km of people in Fiona Fang are irreparably deaf.
From the above power consumption test, we know that the new technology is really helpful to reduce the power consumption of the graphics card (at the same frequency), so can the new technology greatly improve the overclocked ceiling of the graphics card? Let’s do the overclocking test of the graphics card.
We downloaded TRIXX from official website of Sapphire as overclocking software for graphics card, and overclocked the core with a gradient of 50MHz until the graphics card appears abnormal situations such as split screen, blue screen and stuck, and then gradually lowered the frequency at 10MHz. After the core frequency is determined, the memory frequency is properly exceeded in the same way.
The process of overclocking omits 10 thousand words, and finally we put the graphics cardThe core frequency has stabilized at 1650MHz.The overclocking amplitude is 6.8%.The actual frequency of video memory has exceeded 2120MHz.The overclocking range is 6%. The overclocking range of this graphics card really surprised me. Let’s take a look at the performance of the graphics card after overclocking.
1080p
2K
1080p
2K
The higher the frequency of the graphics card of the same specification, the smaller the income after overclocking, but the performance of the graphics card is still improved by about 5% after overclocking, and it is still a little far from touching the GTX 1070 ass. The closest one is 3DMark FSU, which is about 8% different from the GTX 1070 public version.
The cost of overclocking is also quite high. The power consumption of the graphics card has increased by about 60w. Strangely, the power consumption of the platform game is basically the same as that of the baking machine, but it is the same after repeated tests, probably because the frequency of the graphics card in the game is not stable. In short, players who want to overclock should remember to prepare a high-power power supply with good quality. After all, this wattage is almost catching up with RX VEGA 56.
The comprehensive evaluation of RX 590 is here for the time being. I believe that after reading the whole article, everyone will have a more comprehensive understanding of AMD’s new graphics card. Next is your favorite comprehensive performance percentage chart.
Finally, we synthesize the game performance of the graphics card at 1080p/2K and the theoretical performance of 3DMark, and get the above chart.The comprehensive performance of RX 590 with public frequency is about 18% ahead of GTX 1060, and about 11% ahead of ASUS DUAL RX 580 O8G which is close to public performance.
However, the graphics card is still about 25% behind the ASUS DRAGON GTX 1070 TOP8G, and about 37% behind the sapphire RX VEGA 56 ultra-platinum limited edition. However, these are non-public graphics cards, and the reduction of the non-public edition will bring the corresponding performance increase. Xiao Bian roughly estimated that RX 590 is about 16% behind the GTX 1070 public edition and about 33% behind the RX VEGA 56 public edition. Of course, this is only a rough estimate. Please read it.
I prefer to call it RX 580X rather than RX 590.
Previously, the RX 580 high-frequency non-public comparison RX 480 public version has only increased by 13%. Although the RX 590 also adopts the routine of frequency raising, the improvement is more sincere. GF’s 12nm technology can improve the performance of the second generation Ruilong by about 10% compared with the first generation Ruilong, and also improve the performance of RX 590 by about 12% when the power consumption is slightly increased. This 10% improvement is really good in the CPU field, but it is not enough in the graphics card field, not to mention that NVIDIA’s 10-series graphics card has an amazing 70% improvement compared with the 9-series graphics card, even if AMD’s own graphics card is upgraded, such as RX 480 compared with R9 380X.
AMD may also consider this point, and did not give the new graphics card the title of RX 680, but it is the first time that AMD~90 model’s graphics card specifications have not changed ~80 model’s graphics card has not changed. I prefer to call it RX 580X rather than RX 590. (Although RX 580X already exists, it is a RX 580 vest specially supplied by OEM channel.)
Even so, RX 590 is still very competitive in the market.
Having said that, the pricing of RX 590 graphics card is more sincere, and most models are still set below 2000 yuan.Considering that even the public version of RX 590 still has a performance gap of at least about 10% compared with the top non-public version of GTX 1060 6GB.That ticket of GTX 1060 priced at 1900 yuan or above has no purchase value, unless your power supply quality is really poor or wattage is low.
Most models of RX 590 in the market, such as the sapphire RX 590 Ultra Platinum Aurora Special Edition and Dylan RX 590 Demon, are top-level non-public workmanship. In contrast, many GTX 1060 materials of 1800~2000 yuan are very poor, which makes RX 590 more competitive in the mid-range graphics card market.
So is the RX 580 no longer worth buying? Actually, it’s not. Now the price of RX 580 has dropped rapidly. Many beggar versions of RX 580 have dropped to 1599 yuan in JD.COM. Just like GTX 1060, it depends on whether it’s worth buying or not and the actual price.
In the face of the GTX 1070 graphics card, which is currently priced at about 3,000 yuan, Xiaobian can only say that the RX 590 is still fragrant.
It is reported that AMD’s new graphics card will be put on shelves in JD.COM at 10: 00 on November 16th.And the purchase of RX 580, RX 590 and RX VEGA graphics cards on the same day will send Blizzard game cards worth 210 yuan.Interested netizens can pay attention to a wave.
Write it at the end
Although the RX 590 has not improved much this time, AMD’s strategy of running in small steps is quite successful. After all, although high-end graphics cards are the facade, most people buy dessert graphics cards of around 2,000 yuan. Since high-end graphics cards can’t beat them, it is also a smart choice to continue to exert strength in mid-range graphics cards.
Many netizens may think that 2060 is coming soon, and it seems useless to produce this graphics card. However, according to the high cost and pricing strategy of this new generation of NVIDIA graphics cards, Xiaobian guessed that the pricing of the new generation of 2060 graphics cards should be around 2500~3500 yuan, which is no longer a competitive product in the pricing range with RX 590. The competitor of RX 590 should be the current GTX 1060 6GB. As for GTX 1070, both performance and price are not in the same range as RX 590.
In a word, RX 590 is a graphics card for the market, with few technical highlights. If you have any expectations for the development of A-card, you should wait for the release of 7nm game graphics card NAVI next year, when the process of A-card will be rarely ahead of that of N-card, and AMD may also greatly narrow the gap with NVIDIA by virtue of the double progress of architecture and technology.
Dylan DEVIL RX 590
When RX 580 was released last year, Dylan launched the top-end model DEVIL RX 580, and this time is no exception. DEVIL series is commonly known as the devil, which has always represented the top workmanship level of A card and even all graphics cards. The color scheme of red and black and the magic circle have always been the symbol of the devil series.
Dylan’s first DEVIL RX 590 looks basically the same as DEVIL RX 580, continuing the relatively dark design style of the devil, and its face value is online. In addition, the frequency of the graphics card will reach 1575MHz, which is the relatively high frequency RX 590.
Asus STRIX RX590 8G GAMING
As a card manufacturer, ASUS is naturally indispensable. This STRIX RX590 8G GAMING is the RX 590 model launched by ASUS.
I believe everyone is familiar with the appearance of ASUS STRIX graphics card using ancestral radiator. The model released this time is not O8G or T8G, and its performance should be relatively conservative.